Monkeypox vaccination is NOT the ‘only’ answer.
Treatment protocols must take into account terrain, not just the pathogen.
The mainstream media only ever appears to present a single solution to disease: vaccines. What we’re not told is that a pathogen, such as a virus, depends on the terrain it encounters. In this third part of our series, we’ll explore what this means together with possible treatment and prevention strategies for monkeypox, many of which are easily available and accessible.
This is an exploratory article: treatments mentioned below do not constitute medical advice. Please consult with a health practitioner before undertaking a new treatment protocol.
The problem with germ theory
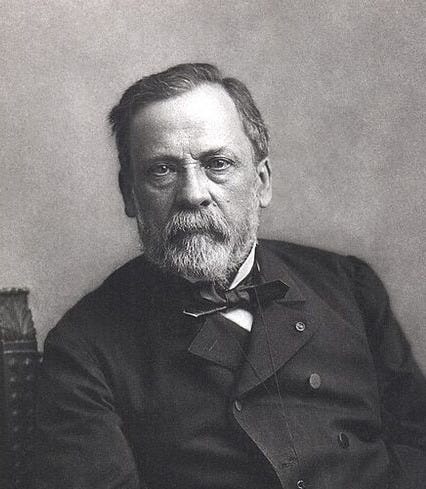
The unshakeable belief that every illness is caused by one microbe is so ingrained in the Western world, that competing ideas about disease causation still have difficulty gaining traction. Louis Pasteur ignored the host and discounted the influence of environmental factors, thereby conveniently dismissing social responsibility for disease.
Our bodies are, in effect, mini-ecosystems. When an individual's internal ecosystem becomes weakened—whether due to poor nutrition, toxicity, or other factors—it can change the function of the microbes that are naturally present in the body, producing disease.
Before looking at treatments that work to bolster the terrain, a word about antivirals.
Antivirals
The CDC states that while some antiviral drugs may help treat smallpox, no treatment has been tested on people sick with the disease. The same is true for antiviral use in mpox. In 2021, the FDA launched a fast-track approval for Tembexa – a drug to treat smallpox. SIGA Technologies, a health security firm whose research was funded by the U.S. government to address the threat posed by biological weapons, has developed an antiviral called Tecovirimat, and this has recently been approved in the US and EU to treat several poxviruses, including monkeypox.
BMJ Best Practice recommends Tecovirimat or the smallpox treatment with Cidofovir or Brincidofovir as the first line antiviral treatment if required, alongside supportive care (including antipyretic, fluid balance, and oxygenation). Empirical antibiotic therapy or Aciclovir may be used if secondary bacterial or varicella zoster infection is suspected. Earlier in 2022, the European Medicines Agency (EMA) approved Tecovirimat for smallpox, monkeypox, and cowpox, caused by viruses belonging to the same family of orthopoxviruses. Interestingly, SIGA stocks have continuously risen since February 2022, while the monkeypox subject was raised in May.
Tranilast
Professor Didier Raoult confirms TRANILAST, a generic medication used in Japan and Korea for allergies and asthma, to be the most effective medicine against monkeypox.
Microbiome
A growing body of evidence indicates that disrupting the homeostasis between the gastrointestinal microbiome and the host immune system can adversely impact viral immunity. A preexisting subclinical infection or peculiarities related to the host microbiome may allow for unabated viral spread in more severe disease cases. So ideally before, but definitely in infection, it is an essential factor in treatment.
Decreasing inflammation
It is generally believed that inflammation is the primary cause of mortality in monkeypox, contributing to fibrin necrotic bronchopneumonia.
There are many ways to reduce inflammation, such as through diet. For example, omitting animal proteins, fats and sugar and grains during an infection, and eating foods such as omega 3 fatty acids, fruit, vegetables, and fermented legumes. There are many anti-inflammatory medicinal herbs to consider: Ashwagandha, Astragalus Root, Calendula, Cat’s Claw, Chamomile, Cilantro, Echinacea, Fenugreek, Holy Basil, Kava Kava, Lemon Balm, Licorice Root, Oregano, Parsley, Passion Flower, Rhodiola, Rosemary, Sage, Spearmint and especially Curcumin in combination with black pepper.
Curcumin (turmeric) and black pepper
This ‘golden spice’ is recognized for its anti-inflammatory, antimicrobial, insecticidal, antimutagenic, radioprotective, and anticancer properties. Over ten thousand studies have reported the biological activities of this compound, including more than 120 clinical trials. Black pepper (Piper nigrum) is widely known for its immunomodulatory, anti-oxidant, anti-asthmatic, anti-carcinogenic, anti-inflammatory, and anti-ulcer properties. Taken together, they have a solid synergistic anti-inflammatory effect.
Psyche and stress
Acute psychological stress has long been known to decrease host fitness to inflammation in various diseases. Interleukin-6 (IL-6) is the dominant cytokine-inducible upon acute stress alone. It has been shown that poor sleep raises IL-6, stressing the importance of including sleep hygiene in health-promoting strategies.
Vitamin D
The inverse relationship between Vitamin D and a pro-inflammatory state has been well-studied. To positively affect immune function, levels of 40-60 ng/mL (100-150 nmol/L) should be reached. As proteins in the progression of monkeypox were shown to influence the Vitamin D receptor, we can assume that they are essential in the progression of the disease.
Zinc and quercetin
Over the past 50 years, abundant evidence has accumulated to demonstrate zinc's antiviral activity against various viruses and via numerous mechanisms. The zinc-finger antiviral protein (ZAP) has been shown to inhibit many RNA and DNA viruses. As the monkeypox virus can lead to health impairments once it has entered the cell, it is advisable to use an ionophore to transport zinc into the cell. An ionophore is an ‘ion carrier’ – a molecule that facilitates the movement of electronically charged ions in and out of cell membranes. Quercetin is an increasingly well-known plant compound with potent anti-inflammatory effects. It works as a zinc-ionophore, increasing intracellular zinc concentrations, and thus, quercetin works as an antiviral.
Sarracenia purpurea
The properties of Sarracenia purpurea, commonly referred to as the ‘purple pitcher plant’, make it a potentially excellent treatment for monkeypox.
Research has shown that a single treatment of S. purpurea caused a 100 to 1000-fold reduction in viral replication throughout the infection, though some viral replication was still observed. In cells treated with fresh extract every six hours, there was a 10,000-fold decrease in VACV replication. In the late 1800’s, the Micmac Indians of Nova Scotia proclaimed the existence of a botanical-based remedy for smallpox. Herbert Miles, the Assistant Surgeon to the Royal Artillery, reported that during an outbreak, “an old squaw going amongst them, and treating the cases with (a botanical) infusion… was so successful as to cure every case”. This botanical infusion was later described as derived from the carnivorous plant sarracenia purpurea. The study, published in the journal PLOS ONE, concluded that “S. purpurea is the only known therapy that will target the virus at this point in the replication cycle.”
Camphor and Borneol
Anastasiya and their team demonstrated the effective use of Camphor and Borneol as potential anti-monkeypox agents.
Yarrow herb
Yarrow is to be taken orally, as in a tea, in the early stages. Yarrow can help break the fever and bring the mpox disease to a speedier ending.
Neem
Neem leaves have been used since ancient times as a natural treatment for smallpox. These work well not only to control infection in a patient but also to prevent spread to others. The paste of neem leaves with water can be applied over blisters to relieve symptoms. If a patient takes a bath, neem leaves can be boiled with water, and a sponge bath can be given to them when they have cooled down. The smoke of neem leaves or hanging fronds of the leaves around the patient helps in curtailing the movement of the virus in the air to protect others.

Artemisa annua
Artemisia annua has demonstrated broad antiviral and immunomodulatory properties that could theoretically be beneficial against monkeypox.
Resveratrol
In a study, resveratrol dramatically suppressed the replication of vaccinia virus (VACV), the prototypic member of poxviruses, in various cell types. Resveratrol also significantly reduced the replication of monkeypox virus. Red grapes, berries, dark chocolate have a high resveratrol content.
Iodine
Dr Pedley has reported the successful treatment of using an iodine solution on the skin lesion for six days twice a day.
Nanosilver
The use of metal nanoparticles provides an exciting opportunity for novel antiviral therapies. Since metals may attack a broad range of targets in the virus, there is a lower possibility of developing resistance than conventional antivirals. The present review (such as here and here), focuses on developing methods for producing silver nanoparticles and their use as antiviral therapeutics against pathogenic viruses.
CDL (chlorine dioxide)
CDL has proven efficient for many viruses and has been recommended by some. More research is needed to make a conclusive statement.
3-Hydroxyphthalic anhydride-modified β-lactoglobulin (3HP-β-LG)
This compound, derived from bovine β-lactoglobulin, is a clinically used anti-human papillomavirus (HPV) agent. It has been found to be highly effective in inhibiting the vaccinia virus infection (a close relative of the monkeypox virus) and the monkeypox virus itself. The compound works by binding to the virus, not the host cell, and preventing the early stages of virus entry. It shows potential for topical application to prevent sexual transmission of the monkeypox virus.
Treatment approaches may vary depending on the severity of the infection, the patient's underlying health conditions, and the healthcare resources available.
In summary
Since monkeypox transmission comes from close contact, it can be easily contained without resorting to a general population vaccination campaign. Since no drug or vaccine is safe, a vaccination program may even be counterproductive.
Disease spread can be readily controlled by classical public health interventions, which include contact tracing, temporary quarantine of those who have had physical contact with someone infected, and more extended-term quarantine of those who develop symptoms.
As outlined in Part 2 of this series, of grave concern is vaccination with a live pox or monkeypox vaccine for people who have had a previous Covid 19 injection, as this has been shown to create so-called VAIDS (vaccine-induced immune deficiency syndrome) with a decline of important Cd 8 cells as well as the profound impairment of Interferon 1 after the injection, which is essential to avoid severe pox and monkeypox complications.
The subversion of innate immunity has been demonstrated. This suppression will have a wide range of consequences, including the reactivation of latent viral infections and the reduced ability to effectively combat future infections. Injecting a live vaccine into an immunocompromised individual not only poses a risk for the individual but can also potentially lead to new virus outbreaks affecting the global population.
Health agencies should halt any attempts to use a live vaccine under these circumstances, considering that almost 70% of the population is said to be Covid 19 ‘vaccinated’. Instead, implementing proven health-promoting steps - so-called lifestyle medicine - could be promoted as a first-line approach. Cost-effective and potent tools such as those covered in this post, could be implemented immediately as a preventative and first-line approach.
In summary, live vaccines are contraindicated for immunocompromised individuals due to the risk of causing disease and spreading the pathogen to other people which could lead to a real explosion of case numbers. It is crucial for healthcare providers to assess the immunocompromised status of patients like Covid 19-vaccinated people carefully and to consider alternative strategies. The World Council for Health stands for a better way and promotes empowerment and not fear.
If you find value in this Substack and have the means, please consider making a contribution to support the World Council for Health. Thank you.






Our greatest danger is now WHOpox. It is the most lethal pathogenic force in history, rivaled only by UNpox.
Thank you, WCH, for this resource. I imagine that timing of some of these products could be important, meaning some for prevention, some for fighting initial virus attachment and entry to cells, some for fighting virus replication, etc. Is there a reference for such instruction to your knowledge?